Why Does My Ankle Hurt?
Explainer video
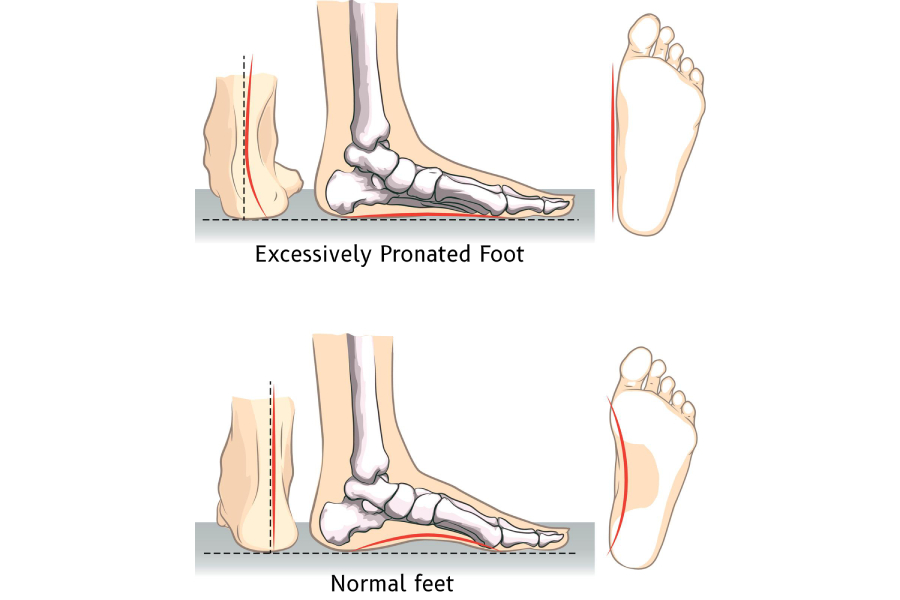
If you have noticed your foot becoming flatter or feel a nagging pain along the inside of your ankle, you aren't alone. You may be experiencing Progressive Collapsing Foot Deformity (PCFD), a condition formerly known as Posterior Tibial Tendon Dysfunction (PTTD). It is the most common cause of "flatfoot" that develops in adulthood.
If you have noticed your foot becoming flatter or feel a nagging pain along the inside of your ankle, you aren't alone. You may be experiencing Progressive Collapsing Foot Deformity (PCFD), a condition formerly known as Posterior Tibial Tendon Dysfunction (PTTD). It is the most common cause of "flatfoot" that develops in adulthood.
Common Signs to Lookout For
• The "Too Many Toes" Sign: When looking at your heels from behind in a mirror, you might see more toes peaking out on the outside of your foot than usual.
• Inner Ankle Pain: You may feel swelling or pain along the path of the tendon that runs behind your inner ankle bone.
• The Heel Raise Challenge: Try standing on one leg and rising onto your toes. If this is painful or impossible, your tendon may be struggling to support your arch.
Who Is Most at Risk?
This condition most frequently affects women in their 50s and 60s. Factors like obesity, diabetes, and high blood pressure can increase the strain on your tendon and make it harder for the tissue to heal.
How Is It Treated?
The good news is that early detection often leads to success without surgery.
• Support: Custom-molded orthotics or special braces (like an AFO) can take the pressure off the tendon.
• Therapy: Shock wave therapy and specific "eccentric" exercises can help strengthen the tendon and your hip muscles to improve your balance.
• Lifestyle: Managing your activity levels and icing can help calm the initial pain.
Disclaimer: The word "treatment" in this article refers to the care and management of a patient’s health to prevent, cure, or improve a condition. Treatment results vary and do not necessarily indicate a cure.
Disclaimer: The word "treatment" in this article refers to the care and management of a patient’s health to prevent, cure, or improve a condition. Treatment results vary and do not necessarily indicate a cure.
For Healthcare Professionals or for a deep dive into the subject matter:
Clinical Perspectives on PCFD: From PTTD to Global Deformity
The transition in nomenclature from PTTD to Progressive Collapsing Foot Deformity (PCFD) reflects a shift in our understanding: this is not merely an isolated tendon failure, but a complex failure of the medial longitudinal arch stabilizers, including the spring and deltoid ligaments.
Updated Staging and Classification
While the Johnson and Strom classification remains widely used, the 2020 Consensus Classification is now the preferred framework. It categorizes the deformity as Stage I (Flexible) or Stage II (Rigid), further subdivided into clinical "Classes":
• Class A: Hindfoot valgus.
• Class B: Midfoot/forefoot abduction (talonavicular uncoverage).
• Class C: Forefoot varus or medial column instability.
• Class D: Peritalar subluxation or sinus tarsi impingement.
• Class E: Ankle instability or valgus tilting.
Diagnostic Nuances
While MRI is frequently viewed as the "gold standard," ultrasound (US) has demonstrated comparable accuracy for detecting tenosynovitis and tears, with the added benefit of real-time examination and lower cost. Clinicians should also be aware of anatomical variations in the tibialis posterior tendon insertion; cadaveric studies show up to four insertion types, with more complex quadruple insertions being highly prevalent in certain populations.
Surgical vs. Conservative Management
Conservative therapy, including eccentric loading and medial arch support, has a success rate of approximately 89% in Stages I and II. However, when surgery is indicated, the goal is joint preservation, especially in younger patients.
• Flexible Deformities: Often managed with FDL or FHL tendon transfers combined with calcaneal osteotomies.
• Rigid Deformities: Typically require arthrodesis (double or triple) to address arthritic changes and stabilize the rearfoot.
Current Research Gaps
There is a notable lack of high-quality randomized controlled trials (RCTs) for non-surgical treatments like shockwave therapy or biologics. Future research is moving toward identifying optimal exercise regimens and validating patient-reported outcome measures like the FAOS specifically for PCFD.
References:
Park, J.H., Kim, D., Kwon, H.W., Lee, M., Choi, Y.J., Park, K.R., Youn, K.H. and Cho, J. (2021) 'A New Anatomical Classification for Tibialis Posterior Tendon Insertion and Its Clinical Implications: A Cadaveric Study', Diagnostics, 11(9), p. 1619. doi: 10.3390/diagnostics11091619.
Rhim, H.C., Dhawan, R., Gureck, A.E., Lieberman, D.E., Nolan, D.C., Elshafey, R. and Tenforde, A.S. (2022) 'Characteristics and Future Direction of Tibialis Posterior Tendinopathy Research: A Scoping Review', Medicina, 58(12), p. 1858. doi: 10.3390/medicina58121858.
Rhim, H.C., Dhawan, R., Gureck, A.E., Lieberman, D.E., Nolan, D.C., Elshafey, R. and Tenforde, A.S. (2022) 'Characteristics and Future Direction of Tibialis Posterior Tendinopathy Research: A Scoping Review', Medicina, 58(12), p. 1858. doi: 10.3390/medicina58121858.
B.T. Pod (SA), MSc (SA)
Podiatrist and Human Gait Specialist
Registered with the Podiatry Association of Singapore
Founder and Director:
Family Podiatry Centre Pte Ltd
Family Podiatry Centre Sdn Bhd
Solescape Orthotics Laboratory
Solescape Shoes brand