Patellofemoral (Runner's Knee) Pain Syndrome

Patellofemoral pain syndrome (PFPS), frequently termed "runner's knee," is the most prevalent cause of anterior knee pain among adolescents and young adults. Characterized by diffuse pain in the retropatellar or peripatellar region, PFPS typically develops insidiously without a specific traumatic event. While the condition is common—affecting approximately 22.7% to 25% of the general population—it is often not self-limiting; nearly 25% of patients report persistent symptoms for more than 15 years after the initial onset. Understanding the role of the foot and the entire kinetic chain is essential to prevent progression toward patellofemoral osteoarthritis.
Pathophysiology: The Pathomechanical Model
The underlying cause of pain in PFPS is widely attributed to elevated patellofemoral joint (PFJ) stress on the outer-side of the knee. This occurs when an imbalance in joint loading disrupts tissue balance, often due to improper tracking of the patella within the femoral groove during weight-bearing flexion (see main image).
Modern research suggests this stress is not merely a local knee issue but the result of a complex interaction between proximal (hip), local (knee), and distal (foot/ankle) factors. Furthermore, chronic PFPS is increasingly associated with pain processing alterations, including local and widespread hyperalgesia (sensitization), indicating that psychological and neurological factors also influence the clinical presentation.
Multi-factorial Etiologies and Risk Factors
The etiology of PFPS is considered multifactorial, involving biomechanical, neuromuscular, and psychological components.
• Quadriceps Weakness: There is strong evidence that reduced knee extension strength is a primary risk factor for future PFPS, particularly in military and athletic populations.
• Proximal Mechanics: Weakness in the hip abductors and external rotators can lead to increased femoral internal rotation and adduction, which directly increases lateral PFJ stress.
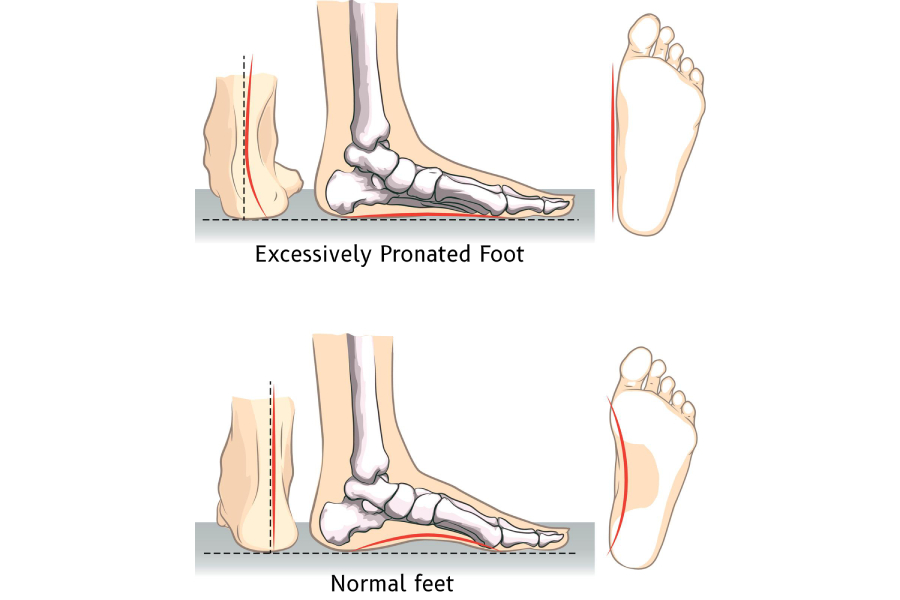
• Foot Factors: Individuals with PFPS often exhibit a more pronated foot posture and increased midfoot mobility. Excessive or prolonged pronation is hypothesized to cause compensatory internal rotation of the tibia and femur, leading to greater dynamic knee valgus.
• Gait Abnormalities: Patients frequently demonstrate reduced gait velocity, decreased stride length, and delayed timing of peak rearfoot eversion during walking and running.
• Psychological Features: Factors such as kinesiophobia (fear of movement) and pain catastrophizing are significantly associated with worse functional outcomes and higher levels of disability.
Clinical Assessment in Podiatry
To effectively manage all contributors to PFPS, clinicians must utilize reliable measurement tools. The Foot Posture Index (FPI), normalized navicular drop, and calcaneal angle relative to subtalar joint neutral (STJN) are both sensitive to group differences and possess high reliability when used by experienced practitioners. For clinical accuracy, pedography foot scans must be used to measure Force-Time curves and other gait parameters that contribute to PFPS.
Evidence-Based Management Strategies
Rehabilitation requires an integrated, multidisciplinary approach tailored to the patient’s biomechanical and psychological profile.
1. Therapeutic Exercise
Exercise is the gold standard of management. Programs that combine hip and knee strengthening (targeting the quadriceps, hip extensors, and abductors) are more effective than knee-focused training alone for improving functional capacity and reducing pain.
2. Foot Orthoses
The use of foot orthoses is a key intervention for patients demonstrating abnormal foot mechanics.
• Mechanisms: Orthoses work by, for example, reducing excessive foot pronation, which corrects the trajectory of the PFJ and minimizes compensatory internal rotation. They also help activate lower extremity muscles, specifically the vastus medialis and gluteus medius, to control lateral patellar movement.
• Clinical Effectiveness: Meta-analyses show that orthoses significantly improve knee function and sport-related performance.
3. Radial Shockwave Therapy (ESWT)
• Biological Stimulus: ESWT provides a mechanical stimulus that triggers mechano-transduction, promoting tissue regeneration, collagen synthesis, and reduced inflammation.
• Functional Gains: Studies indicate that adding ESWT to standard programs results in superior pain reduction, improved joint mobility, and increased muscle mass (quadriceps volume), likely because pain reduction allows for higher-intensity exercise participation.
4. Adjunctive Modalities
Other interventions that can provide short-term relief to facilitate exercise include patellar taping (McConnell taping), manual therapy, and gait retraining. Gait retraining, specifically, can help reduce frontal plane hip motion and improve overall lower-limb mechanics.
Conclusion
PFPS management must move beyond treating the knee in isolation. Successful outcomes are achieved by restoring quadriceps and hip strength, correcting distal biomechanics through foot orthoses, and utilizing advanced modalities like radial shockwave therapy to stimulate tissue healing and improve functional capacity.
Disclaimer: The word "treatment" in this article refers to the care and management of a patient’s health to prevent, cure, or improve a condition. Treatment results vary and do not necessarily indicate a cure.
Disclaimer: The word "treatment" in this article refers to the care and management of a patient’s health to prevent, cure, or improve a condition. Treatment results vary and do not necessarily indicate a cure.
References:
Neculăes, M., Hernandez-Lucas, P., Ioja, I.B. and Lucaci, P., 2024. Contribution of Shockwave Therapy in the Functional Rehabilitation Program of Patients with Patellofemoral Pain Syndrome. Journal of Clinical Medicine, 13(23), p.7260.
Written and prepared by:
Mark Reyneker
Written and prepared by:
Mark Reyneker
B.T. Pod (SA), MSc (SA)
Podiatrist and Human Gait Specialist
Registered with the Podiatry Association of Singapore
Founder and Director:
Family Podiatry Centre Pte Ltd
Family Podiatry Centre Sdn Bhd
Solescape Orthotics Laboratory
Solescape Shoes brand